Abstract
Introduction: The rapid availability of SARS-CoV-2 mRNA vaccines at the beginning of 2021 allowed to a relative protection of recipients of allogeneic stem cell transplantation (Allo-SCT) since up to 80% of patients developed anti-spike (anti-S) antibodies after two doses. In addition, cellular adaptive responses have also been documented after 2 shots. For example, we recently reported a strong response of specific anti-SARS-CoV-2- CD4+ T-cells, with a IFNγ-/TNFα+ cytokine profile, in 89% of humoral responders and 40% of non-humoral responders (Clemenceau, 2022). The interest of at least one booster has been confirmed thereafter with a persistent and significant reduced incidence of severe form or death due to COVID-19 infections. In this study, we have evaluated humoral and T-cell responses after one (Vaccine 3 or V3 group n=40) or two (Vaccine 4 or V4 group n=12) BNT162b2 mRNA vaccine boosters in 52 Allo-HSCT patients and in 12 healthy donors (only one booster).
Methods: Blood samples were collected between January 18th and March 3rd 2022 during the Omicron wave in France. Anti- spike antibodies were tested using anti-SARS-CoV-2 immunoassay Elecsys® (Roche, Rotkreuz, Switzerland). Anti-SARS-CoV-2 Spike and anti-EBV (as positive control) specific CD3+ T-cell responses were evaluated using Human INFg ELIspot (Mabtech 3420-2AST-10, Nacka Strand, Sweden) and intracellular cytokine staining after peptide stimulation (PepTivator Prot_S Complete, Miltenyi Biotec, Bergisch Gladbach, Germany).
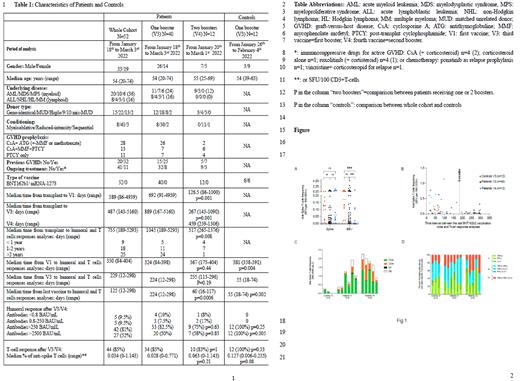
Results Characteristics of the participants are summarized in Table 1. All controls (100%) and 81% of the whole patient cohort have developed a protective anti-S antibody level (>250 BAU/mL) after the boost vaccinations. The rate of subject reaching the highest antibody concentration (>2500 BAU/mL) was significantly higher in controls than the whole patient cohort (100% vs 52%, p=0.005) (Table 1).
After the booster vaccination, 85% of patients and 100% of controls developed a specific-T cell response. Median frequency of anti-Spike T-cells was significantly lower for V3 patients (median: 0.028 spot forming units (SFU)/100 CD3+ T-cells, range 0.000-0.771) than in controls (median: 0.127 (range (0.006-0.235) (p=0.03) but not significantly different between V4 patients and V3 controls (p=0.03) (p=0.08) (Table 1 and Figure 1.A). We did not find a significant difference in the anti-SARS-CoV-2 T-cell frequency between patients whose analysis was done before 6 months after the last vaccination or those for whom the analysis was done after 6 months (Figure 1B). For 14 individuals with the highest frequencies of anti-Spike CD3+ T cells (³ 0.180 SFU/100 CD3+ T-cells), the Th1 cytokine profiles of CD3+, CD4+ and CD8+ T cells were performed by INFg, TNFa and IL-2 intracellular staining. A predominance of anti-spike CD4+ T-cell response was observed and, interestingly, a polyfunctional cytokine profile was observed in both controls (n=3), and patients (V3 n=6; V4 n=5) (Figure 1 C and D).
The only factors predicting T-cell response in patients were CD8+ and NK cells counts at time of analyses. Surprisingly, higher counts were associated with no T-cell response. A good humoral response was not predictive of T cell response (75% vs weak response 82%, p=1).
Importantly, considering the patients with no antibody response (n=5) or not reaching a protective antibody level after boosts (n=5), 8/10 (80%) had a measurable T-cell response.
At time of last follow-up (June 1st 2022), 2 controls with a good humoral and T-cell response (0.125 and 0.235 SFU/100 CD3+ T-cells) have presented a non-severe COVID 19 infections. Similarly, two V3 patients presented with a non-severe form (negative serology and 0.039 SFU/100 CD3+ T-cells and serology >2500 BAU/mL and 0.040 SFU/100 CD3+ T-cells). One V3 patient with negative serology and 0.367 SFU/100 CD3+ T-cells at time of analysis have died of COVID-19 infection.
Conclusion: In this cohort after one or two booster vaccination, 81% of patient achieved a protective humoral response while 85% achieved a T-cell response. T-cell frequencies were comparable between V4 patients and controls while COVID-19 infections were only observed in individuals with one booster. Although these results have to be confirmed on a larger cohort, it may indicate that two booster vaccines may help to achieve sufficient protection in allotransplanted patients through a persistent specific T cell response.
Disclosures
Chevallier:Pfizer: Research Funding; Abbvie: Honoraria; Jazz Pharmaceuticals: Honoraria; Takeda: Honoraria; Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal